News
Stroger Hospital slammed for plan to merge pediatric, adult emergency rooms
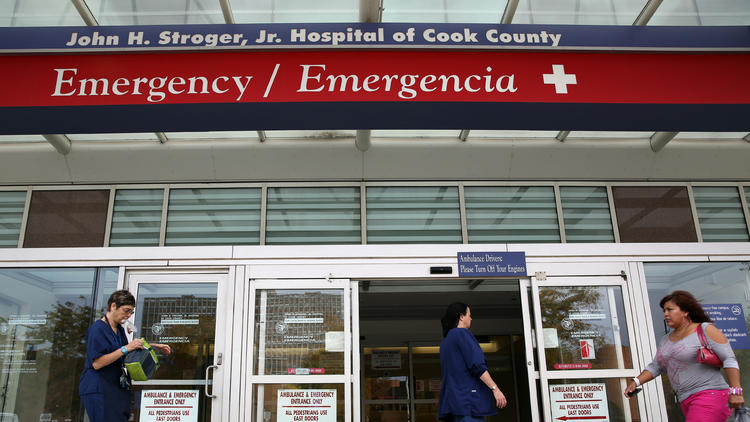
IMAGE CAPTION
CAPTION
-->At Cook County board meeting this month, Dr. Tatyana Kagan stood to address the commissioners. It was the first time she had attended a meeting.
Kagan works in the pediatric emergency room at Stroger Hospital and came to object to the hospital's plan to consolidate the pediatric ER with the main ER.
Reading from a speech, Kagan said the creation of a single emergency department would harm quality of care, subjecting children and their guardians to long waits and the sometimes chaotic atmosphere of the adult ER.
"Emergency departments are not one-size-fits-all," Kagan told the commissioners. "Babies are not mini adults. They require specialized care that only a pediatric emergency room can provide."
Kagan was one of several doctors and nurses at Stroger who protested the planned ER change as well as other plans by the Cook County Health and Hospitals System to reorganize the hospital's pediatric services.
The changes are being made to adapt to a lower volume of pediatric cases, said Dr. Jay Shannon, chief executive of the county health system. The hospital plans to make the service changes before the end of the year.
"It's part of the ongoing organic nature and good management of space and facilities and patient care that you are constantly in a state of dynamism where you're trying to flow services to where you need them the most," Shannon told commissioners.
The controversy underscores the challenges facing safety-net hospitals like Stroger in a new era of health reform. Hospitals are under intense pressure to become more efficient as part of a transition from the traditional fee-for-service reimbursement system to one that rewards hospitals for good outcomes and controlling costs.
But for safety-net hospitals, the need for efficiency can sometimes clash with their public missions.
Stroger has long played a special role in Chicago's health care system by serving large numbers of low-income, uninsured and socially vulnerable patients regardless of their ability to pay. As a provider of last resort, the public hospital is expected by the community to offer comprehensive services, even if some of those services are not profitable. To offset unreimbursed or under-reimbursed care, the county government provides supplemental funds to the health system.
The Affordable Care Act has brought significant changes to the county health system. For one, more of its patients have insurance. Thanks to the expansion of Medicaid, about two-thirds of its patients are insured, up from 45.6 percent in 2013. As a result, the amount of uncompensated care shrank to $340 million last year, from more than $500 million in 2013.

Dr. Tatyana Kagan, who works in the pediatric emergency room at Stroger Hospital, said the creation of a single emergency department would harm quality of care, subjecting children and their guardians to long waits and the sometimes chaotic atmosphere of the adult ER. (Jose M. Osorio / Chicago Tribune)
Dr. Tatyana Kagan, who works in the pediatric emergency room at Stroger Hospital, said the creation of a single emergency department would harm quality of care, subjecting children and their guardians to long waits and the sometimes chaotic atmosphere of the adult ER. (Jose M. Osorio / Chicago Tribune)
The health system also started an insurance business. It set up a managed care plan to serve Medicaid beneficiaries in Cook County, which has helped stabilize the system's finances.
The move into insurance also means the health system has to compete with other Medicaid plans to retain and grow its membership of about 170,000. A lot of its members are newly insured and for the first time have a choice of doctors and hospitals. They no longer have to depend on Stroger or the system's other medical centers and outpatient clinics for their care.
In this competitive environment, Shannon sounds like a football coach. "We've got to up our game," he said during a recent visit to the Tribune's editorial board.
The CEO said that means delivering services based on market demand and the health system's expertise. When Shannon, who has been the chief executive since January 2014, looked at the demand for pediatric services at Stroger, the trends didn't look good, he said.
Between 2004 and 2014, pediatric admissions dropped from 1,325 to 494, a 62.7 percent decline, according to state data. The occupancy rate, based on licensed beds, has declined from 49.9 percent to 15 percent over the same period.
Visits to the pediatric emergency room by kids 17 and under fell 21.2 percent, to 6,104, between 2010 and 2014, according to data provided by the health system. Total ER visits at Stroger declined 5 percent over the same period. Kids made up only 5.2 percent of all emergency visits at Stroger last year.
Shannon said the decline in pediatric admissions is a public health victory — a reflection of higher vaccination rates and better antibiotics. With healthier children, a lot of pediatrics care has shifted away from hospitals to outpatient settings in Chicago and across the nation, said Mark Wietecha, president and CEO of the Children's Hospital Association in Washington.
Stroger's pediatric trends are reflected across Illinois hospitals. Pediatric admissions have declined 22 percent since 2007, according to the most recent state data. Hospitals have responded by reducing the number of beds by 30 percent and partnering with children's hospitals and academic medical centers that have more specialists on staff. In the Chicago area, for instance, Lurie Children's Hospital runs inpatient pediatric services at several hospitals, and University of Chicago Medicine provides pediatric specialists to Edward-Elmhurst Health in the western suburbs.
Shannon acknowledges another reason for the decline in pediatric admissions at Stroger in the last decade. In 2005, then-Gov. Rod Blagojevich signed legislation to expand Medicaid to cover more children.
As a result, parents went to other hospitals typically closer to their homes, Shannon said. But the loss of volume since 2006 also means something else, said Nancy Kane, a management professor at Harvard University's T.H. Chan School of Public Health.
"That says something about the perception of quality at Stroger," Kane said. "Parents have choices and talk with their feet."
Shannon, who worked at Stroger and its predecessor, Cook County Hospital, for 17 years, doesn't hide from shortfalls at Stroger and the rest of the health system. He ticks off a list of areas where the system could improve its customer service: adding parking, expanding clinic hours, updating facilities and hiring more bilingual staffers.
To pay for those improvements, the hospital would like to generate capital from improvements in operations, said Doug Elwell, deputy CEO for finance and strategy.
"I can assure you we are looking at the dollar value of everything we're doing," Elwell said at the editorial board meeting. "There are some things that we will look at and say if it's available in the community and we can't do it at a reasonable financial investment then we're not going to be able to do it. We're going to have to staff to the volumes we can do and what we can do and do it well."
Doctors and nurses say they understand the need for a more modern and financially healthy system but said it shouldn't come at the expense of children. Cutting back on inpatient pediatric care will affect demand for other services, they said.
"Women are the traditional health care decision-makers in every family," said Dr. Richard David, co-director of the neonatal intensive care unit at Stroger. "If they can't get obstetrical or pediatric care in our hospital, why would they bring their ailing parents here?"
David and other doctors also have criticized Shannon for not being transparent about the changes he would like to make. They said they were not consulted about the pediatric plans and first heard about them in the media.
In a strategic planning update on Sept. 22, Shannon said the hospital will designate exam rooms in the main emergency department to accommodate children under 18. Stroger also plans to consolidate the 40-bed inpatient pediatric unit with the 10-bed pediatric intensive care unit. The hospital is finalizing how many beds will be in the combined unit, a spokeswoman said.
In addition, patients 18 and over, which represent one-quarter of inpatient volume, will be cared for on adult floors, Shannon said in the update.
While reorganizing pediatric services at Stroger, Shannon would like to expand the services children receive in their communities.
He said it can be difficult for a child on Medicaid to see a cardiologist, neurologist or an endocrinologist. Shannon would like to reuse the space devoted to inpatient care at Stroger and turn it into outpatient care for moms and their kids. Some of those outpatient services are provided at the Fantus Clinic, across the street from Stroger, but Shannon would like to close the facility, calling it "abysmal." He also has ambitious plans to build an ambulatory center near the system's Provident Hospital on the South Side.
"We have a significant problem with health care disparities in this region," Shannon said at the board meeting. "We believe we can improve that by improving our primary care service both to children and expectant mothers and by growing access to needed ambulatory specialty services to children."
While Shannon is the target of several critics, Harvard's Kane said she sympathizes with the difficult task ahead of him under the Affordable Care Act.
"All hospitals, including safety-nets, increasingly have to ask themselves what do I do really well," she said. "No one has infinite resources."