National Nurses United urges the CDC to revise its dangerous guidance saying vaccinated people no longer need to wear masks, get tested, or isolate after an exposure

The science does not back up abandoning public health infection control measures on wearing masks, distancing, testing, and quarantining based on vaccination status.
On May 13, the Centers for Disease Control and Prevention (CDC) issued updated guidance for fully vaccinated people, stating that they no longer needed to wear masks in any settings besides health care and public transportation, no longer needed to distance from others outside their households, and no longer needed to quarantine themselves or get tested if they have been exposed to Covid-19 but don’t show symptoms.
National Nurses United strongly condemns this dangerous guidance that puts nurses, other essential workers, children, and medically vulnerable people at risk and demands that the CDC revise it to continue requiring these multiple infection control measures in our fight to control Covid-19. You can read our statement here.
We are also issuing a scientific brief that analyzes the faulty science behind this CDC guidance and explains the science showing multiple measures are still needed to curb Covid-19. You can download and read the full brief here, but we provide highlights below.
The basics: How the virus spreads should determine what public health measures will work.
- The virus spreads through aerosol transmission. When an infected person speaks, breathes, coughs, or sneezes, they release tiny particles containing infectious virus. These aerosol particles can travel long distances and stay suspended in the air. When another person breathes in these particles, they can become infected.
- The virus can be transmitted by people who are infected but show no symptoms. They are either asymptomatic or have not yet developed symptoms. Studies show up to half of Covid-19 transmissions are by people with no symptoms.
Study after study shows that multiple measures, including masks, are needed to stop the spread of Covid-19.
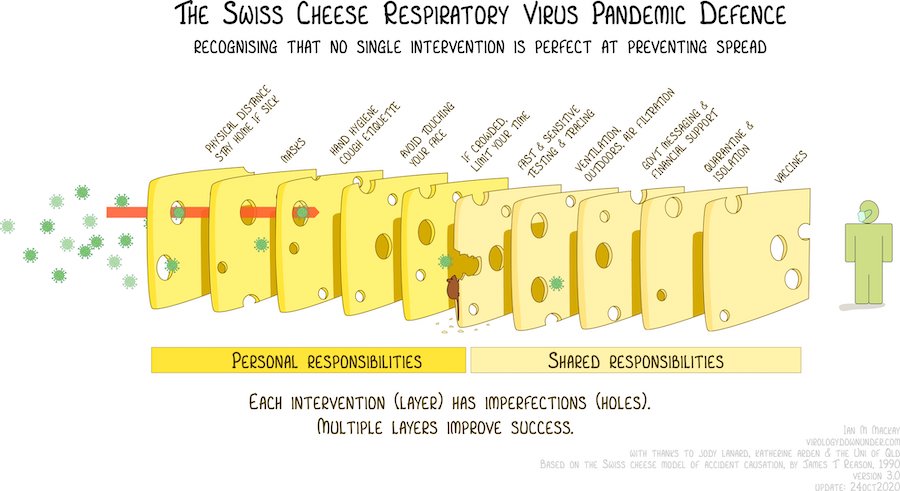
Think of each infection control measure as a slice of swiss cheese with holes. Each slice, or measure, by itself could allow the virus to pass through its holes. But if you stack multiple slices together, you can prevent the virus from passing. Vaccines represent just one slice of cheese in this scenario. We must include distancing, testing, contact tracing, and quarantining.
Covid-19 vaccines are effective at preventing serious infections, hospitalizations, and deaths in a majority of people, but we cannot depend on vaccination alone. First, just over 37 percent of people in the United States have been fully vaccinated. Children under 12 years do not have access to a vaccine currently. Second, no vaccine is 100 percent effective. Third, there are still many unknowns about vaccines, including how long immunity lasts, whether they work against the proliferating number of Covid variants circulating, and if they prevent transmission by vaccinated, infected people with mild or asymptomatic cases.
Additionally, the CDC announced last week that it is no longer tracking cases of “breakthrough infections,” meaning people who have been vaccinated but still get infected, unless they lead to hospitalization or death. In short, the CDC simply is not collecting the data needed to know whether its recommendations for vaccinated people hold true.
Widespread masking is a simple, cheap, and highly effective method for preventing the spread of the virus, and must be combined with other measures.
Because such a high percentage of Covid-19 cases are asymptomatic, testing, contact tracing, and quarantining are also critical components of infection control. It’s not good enough to only prevent Covid-19 cases that lead to hospitalization or death. We must dramatically lower infection numbers to stop the virus from further mutating, and also aim to prevent mild or asymptomatic cases which have been shown to lead to other negative long-term health consequences.
The CDC’s recent guidelines irresponsibly put at risk nurses and other essential workers, who are disproportionately people of color, as well as children under age 12, babies, and medically vulnerable people who do not qualify for vaccination.
The CDC appears to have based its guidance upon real-world vaccine efficacy data that is incomplete. Many of the studies cited were either not yet peer reviewed, were conducted by people with a conflict of interest or by a vaccine manufacturer itself, or reported poor statistical certainty in the findings.
The science is clear: Given what we know and what is still unknown, we must take the safety-first route to protect public health by maintaining multiple measures of infection control, including masking, while at the same time working harder to increase vaccination rates. Depending upon faulty science won’t increase vaccination rates; extensive public education and making vaccines truly accessible for working people and underserved communities will.