News
Widespread Understaffing of Nurses Increases Risk to Patients
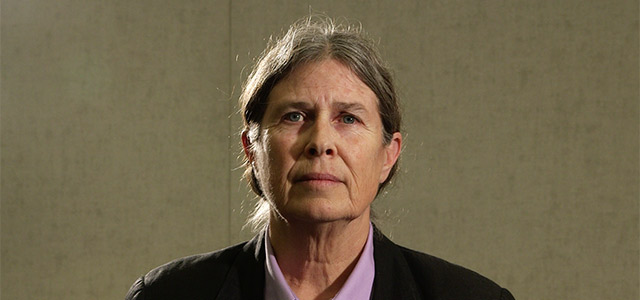
Over her 34-year nursing career Martha Kuhl, a pediatric oncology nurse at U.C.S.F. Benioff Children’s Hospital Oakland in California, has seen her patient load more than double. She recalls one night shift when she was the lone nurse on duty with five patients. “These are all babies that can’t breathe,” she says. “I felt okay at four” but that last patient “sort of tipped it over the edge where I felt unsafe in being able to handle all of these patients.”
Kuhl’s description sounds like a worst-case scenario, but in fact she can recall several similar times where “it was impossible to give proper care” due to understaffing. Mounting data from hospitals nationwide are proving Kuhl correct: When staffing levels fall below certain nurse-to-patient ratios, the patients are more likely to suffer or even die.
In hospitals things tend to snowball. Patients there are already at a high risk for something to go wrong. “It’s sort of like planning for any potential disaster‑ it’s not a matter of if, it’s when,” says Bonnie Castillo, director of the Registered Nurses Response Network at National Nurses United (NNU), a nurses’ union. “If you have several patients, and one is having a sudden hemorrhage and one is having chest pain and the other is having a stroke or is choking, you have to have enough nurses that can deal with each of those instances and not place one above the other.”
Yet many nurses in the U.S. and worldwide say they are forced to make those uncomfortable assessments on a daily basis because hospital administrators do not want to spend the money needed for ample staffing. The popular press usually attributes the chronically overburdened state of American hospitals to a national nursing shortage, but most everywhere there has been a surplus of educated nurses for years, according to the U.S. Health Resources and Services Administration. “We have more nurses in the U.S. than we’ve ever had before,” says Linda Aiken, director of the Center for Health Outcomes and Policy Research at the University of Pennsylvania. “It’s really the lack of budgeted positions in hospitals.”
Hospital administrators are reluctant to hire more nurses because it is not seen as cost-effective, Aiken says. However, “it’s costing more to not have adequate staffing because of all these excess costs that they are getting from these poor outcomes,” such as patients who return, postsurgical infections and other consequences of short staffing.
With the advent of better collection and monitoring of health care data, recent research supports nurses’ assertions that understaffing has a cascading effect on hospital outcomes. In a study this March in Critical Care Medicine comparing a diverse group of hospitals worldwide, a higher nurse-to-patient ratio correlated with lower patient deaths in intensive care units, for example. Another study published inThe Lancet in 2014 found that an increase in a nurse’s workload by one patient increased the likelihood of a patient in that hospital dying by 7 percent. “In every single country, and states within countries, there’s a tremendous variation in nurse staffing in hospitals that cannot be explained on the basis of how sick patients are or any other reasonable explanation,” Aiken says. “And along with that variation in nurse staffing is variation in every other patient outcome, from mortality to falls with injuries, to patient safety events to patient satisfaction.”
California is one of the few states to regulate hospital staffing, and the only one to set minimum nurse-to-patient staffing ratios—ceilings for how many patients a nurse can be held responsible for at a time, which vary by unit. The law, enacted in 2004, has provided an interesting test-case for the effects of mandatory staffing ratios.
The California experience ties staffing ratios to various improvements in patient care, including lower rates of postsurgery infection, falls and other micro emergencies in hospitals. In a 2014 study commissioned by the Agency for Healthcare Research and Quality, part of the U.S. Department of Health and Human Services, researchers compared hospital care utilization and financial data in California, Maryland and Nevada. After the law went into effect California patients experienced fewer adverse events than the others, although the effect was moderate. Patient length of stay in the hospital, however, was reduced significantly, a finding that has been replicated in other studies.
Staffing ratios also appear to reduce the rate of readmissions, many of which are preventable and constitute a significant cost for hospitals. The Affordable Care Act (ACA) sets penalties for hospitals with high rates of readmissions. In one 2013 studyresearchers at the University of Pennsylvania School of Nursing examined data from hospitals across the U.S. and found that those with higher staffing ratios had 25 percent lower odds of being penalized under the ACA for excessive readmissions than ones with lower staffing ratios but otherwise similar conditions. Another study that year also from the same school examined 30-day readmissions in California, New Jersey and Pennsylvania and found that each additional patient per nurse raised readmission rates 6 to 9 percent.
The effects of staffing are most pronounced with patients at the highest risk. In 2011 study published in Health Services Research, Aiken and colleagues compared California with New Jersey and Pennsylvania. California hospitals had 14 percent fewer postsurgical deaths than New Jersey and 11 percent fewer than Pennsylvania, when matched for variables other than staffing ratios. The start of staffing ratios was associated with rapid decreases in mortality rates but even more in “failure to rescue”—the capacity of a hospital to save the life of a patient who experiences a complication. This is a more sensitive measure of nurse impact, looking at the survival rates of patients that develop a complication rather than patient death overall, Aiken says. “Nurse staffing is very highly related to that.”
Other studies have found that patients in better-staffed hospitals use fewer intensive care unit days, another big source of cost.
Nurse-to-patient ratios have also had an immediate impact on occupational injuries, many of which are the result of patients physically assaulting nurses. The rate of workplace injuries to nurses “dropped right away,” says J. Paul Leigh, lead researcher and professor of health economics at University of California, Davis. This May Leigh and colleagues published a paper reporting that the injury rate in California went down 32 percent, more than in the other 49 states after the law.
The California ratios are determined on the basis of patient acuity, or how severe their case is. By basing nurse staffing on this metric, those patients “are able to get the level care they need rather than falling through the cracks,” improving several types of outcomes, says Castillo of NNU, the driving force behind the California law. “You can’t have a situation where you have four or five kids and they are all” at the extreme end of the severity scale, agrees Bridgitt Manson, a nurse for 28 years, currently at the University of Chicago Medical Center (UCMC) Comer Children’s Hospital.
Other states are now considering regulation of hospital staffing, and there is a bill before Congress to federally implement staffing ratios in hospitals. Nurses’ groups have faced strong opposition from hospital administrations, however, especially against mandated nurse-to-patient ratios. In 2008 Illinois enacted a law requiring hospitals to develop staffing plans built around acuity and the complexity of the patients’ needs, but it stopped short of California’s mandated ratios.
Manson is the co-chair of the nursing acuity committee at the UCMC, which makes quarterly staffing recommendations to the administration for different hospital units, based on experience and data about patient acuity, quality of care and other factors. “We have an abundance of staffing issues,” even after the law, Manson says. She struggles to recall a single instance in which the UCMC administration has adjusted staffing based on the nurses’ acuity assessments in the seven years in which she has served on the committee. “Nurses are filling out these forms and the recommendations are going on deaf years,” she says. “They’re not going by the tools that they built,” she says of the hospital administration. “Acuity is supposed to guide staffing, not a staffing matrix, and that’s not what’s happening.”
In April UCMC nurses threatened to strike over hospital staffing, before reaching a tentative deal. Chief Nursing Officer Debra Albert, a UCMC administrator, acknowledges there are situations in which recommendations are denied based on factors “not captured in an acuity system,” such as the general level of activity on the unit. The UCMC is against nurse-to-patient ratios because they “don’t provide flexibility to staff based on patient need, they provide a one-size-fits-all staffing model,” she says.
Her response echoes that of many other hospital associations when discussing nurse-to-patient ratios. Nurses’ groups say they agree on the need for flexibility, however. “The way the laws are written, we have no problem flexing up,” Castillo says. But hospitals have a history of stretching the limit of what’s safe. “This is not like any industry where we are dealing with inanimate objects. We are dealing with human lives.”