Mpox Virus Transmission: Review of the Scientific Evidence

- Introduction
- About the Mpox Virus
- Evidence on Transmission Modes of MPV
- Transmission in the Absence of Symptoms
- Other Transmission Modes
- Additional Considerations for Transmission
- Citations
Introduction
Since early 2022, the mpox virus (Clade II) has spread rapidly around the world. In 2024, a different clade of mpox (Clade Ib) has surged in several countries in Africa. As with any infectious disease outbreak, the methods of transmission determine which protective measures are needed. Many pathogens spread via multiple transmission methods at the same time, requiring multiple layers of protective measures to contain spread.
Where there is scientific uncertainty, the precautionary principle states that the highest level of protection should be chosen in order to prioritize protecting people’s health. This document summarizes the current scientific evidence—and unanswered questions—regarding the transmission modes of the mpox virus.
About the Mpox Virus
Human mpox is a zoonotic viral disease caused by the mpox virus, which belongs to the same family of viruses as smallpox. The first human case was identified in 19701. Mpox is considered a re-emerging disease that has caused multiple localized outbreaks since 2017. The mpox virus is now spreading rapidly in many countries that have not historically had cases.
There are two clades of mpox virus: Clade I and Clade II. Clade I virus (including subclades 1a and 1b) can cause more severe disease and has a higher mortality rate (about 10 percent). Clade II causes less severe illness and 99.9 percent of people survive infection. The outbreak in 2022 was caused by Clade II mpox virus. The surge in cases in 2024 is caused by Clade Ib.
Animal-to-Human Transmission
While the natural reservoir for the mpox virus has yet to be determined, the virus has a wide range of animal hosts, including prairie dogs, squirrels, wild chimpanzees, shrews, monkeys, dogs, and Gambian pouched rats.2,3,4,5,6 Mpox-infected animals can have similar clinical manifestations to humans infected with the virus, including respiratory signs of varying severity and skin lesions that range from one to several. Studies have also shown that saliva, urine, and feces from infected animals can contain viable mpox virus.7,8 Animal-to-human transmission of mpox has been documented through contact and airborne transmission routes.9 For example, occupationally transmitted infections occurred in several veterinary staff during the 2003 U.S. mpox outbreak while handling or caring for mpox-infected prairie dogs within six feet.10
Human-to-Human Transmission
Human-to-human transmission of the mpox virus, including nosocomial and household transmission, has been well documented.11,12,13 For example:
- Health care workers were infected during the 2017-18 outbreak in humans in Nigeria.14
- Between 2018 and 2021, seven mpox cases were identified in the UK, two of whom were infected in a household cluster with a travel-associated case and the other was a health care worker who was infected after caring for the patient without PPE.15
Human-to-Animal Transmission
Human-to-animal transmission of mpox has also been identified during the 2022 outbreak. A pet dog developed lesions and tested positive for the virus, twelve days after its owners developed symptoms of mpox.16 The dog shared a bed with both owners but had not had contact with other pets or other humans.
Evidence on Transmission Modes of MPV
Contact Transmission
Main points:
- Most patients infected with mpox virus present with infectious skin lesions.
- Mpox virus can remain infectious in the environment at least 15 days, possibly longer, primarily on porous surfaces (e.g., bedding and clothing).
- Mpox virus has been detected on many surfaces in houses and hospital rooms of positive patients.
Contact transmission of the mpox virus is well established. Infection with the mpox virus typically results in skin lesions, with 95 percent of patients presenting with rash.17 Research has shown that 99 percent of skin lesion swabs were positive for mpox,18 and that skin lesions had the highest positivity rate and viral load of specimens tested.19,20 Contact with lesions of an infected patient is thought to be one primary transmission mode for the mpox virus. The virus can enter the body through mucous membranes and broken skin.
The mpox virus is an orthopoxvirus, which has exceptional ability to remain infectious in the environment.21 Viable (infectious) mpox virus has been found on surfaces from households where an individual with mpox left up to 15 days prior to sampling. Viable virus was detected primarily on porous surfaces, such as bedding and clothing.22,23
Research has documented extensive environmental contamination with the mpox virus.24,25 For example, patients with mpox infections were isolated in hospital rooms and viral contamination was found on sink handles, soap dispensers, toilet seats, chair surfaces, mobile phones, cabinet doors, fabrics used by the patients, gloved hands of the investigators, and all hand-contact points in the anteroom.26 Infectivity was demonstrated for some surfaces, including gloves, after handling contaminated fabrics.
During the 2003 mpox outbreak in the United States, researchers found that human mpox cases were likely associated with daily exposure to infected prairie dogs through touching and/or cleaning cages and soiled bedding.27 This study highlights that potential exposure to excretions and secretions of an infected prairie dog (e.g., urine, feces, and saliva) could have led to transmission.
Unanswered questions:
- What is the viral load required to cause an infection?
- Can patients without lesions shed infectious virus? How?
- Can transmission occur via other bodily fluids (e.g., urine, feces, saliva, semen, vaginal fluid, blood, etc.)?
- Can infection occur via inoculation in the eye? Via ingestion?
Airborne/Aerosol Transmission
Main points:
- Studies show that airborne/aerosol transmission of mpox is possible and has likely occurred, though it is unclear how often it happens.
- Mpox virus is stable suspended in aerosols for at least 90 hours.
- Mpox virus can be aerosolized when contaminated objects, such as bedding and clothing, are moved and shaken.
Mpox virus can be aerosolized during viral shedding in the respiratory tract and/or through lesions of the mouth or throat during breathing, speaking, coughing, or sneezing. Airborne/aerosol transmission potential of the mpox virus is also well established. While the scientific literature indicates that airborne/aerosol transmission may not be the predominant or most frequent mode of transmission for the mpox virus, scientific evidence shows that it is possible and has occurred. Therefore, measures to prevent airborne/aerosol transmission of the mpox virus are necessary.
There are two primary ways that the mpox virus may become airborne:
- Infectious virus that is present on objects, such as bedding and clothing, can become aerosolized when the object is moved, especially if it is shaken.
- People who are infected with the mpox virus shed virus in their respiratory tracts and can have lesions in their throats and mouth. Virus can become aerosolized when people breathe, speak, cough, sneeze, laugh, or sing.
Like other orthopoxviruses, the mpox virus has an exceptional ability to remain infectious in the environment for long periods of time. One study found that the virus was viable (infectious) after 90 hours suspended in aerosols.28
Infectious mpox virus that is present on objects, such as bedding and clothing, can become aerosolized when the object is moved, especially if it is shaken.
Objects, such as bedding and clothing, can become contaminated with infectious mpox virus (see section on Contact Transmission), and this virus can be aerosolized when the object is moved. A majority (75 percent) of air samples were positive and 50 percent were viable (infectious) during a bed linen change in a hospital isolation room where a patient with mpox was isolated.29 At least one case has been documented where a health care worker was infected while changing the bedding and clothing of a patient with mpox.30 Because the patient had not yet been identified as having mpox, the health care worker was wearing only a disposable apron and gloves, with no respirator. Similarly, in the 2003 outbreak in the United States, a study found that cleaning the cages or bedding of mpox-infected animals was associated with acquiring mpox.31
Airborne transmission during PPE doffing is of particular concern for health care workers. One study found positive contamination in the breathing zone of a worker while doffing PPE, including a powered air purifying respirator (PAPR), isolation gown, inner and outer gloves, and boot covers, in addition to contamination on the skin on the hands and wrists.32 While a trained observer and doffing assistant were utilized, contamination was observed on every subject to a certain extent.
People who are infected with the mpox virus shed virus in their respiratory tracts and can have lesions in their throats and mouth. Virus can become aerosolized when people breathe, speak, cough, sneeze, laugh, or sing.
Animals and humans infected with mpox and other poxviruses33 can generate respiratory aerosols.34,35 Mpox can cause lesions in the respiratory tract, including on the tongue, in the mouth, and in the throat.36,37,38,39,40,41 Data indicate that about 30 percent of patients have oropharyngeal mucosal lesions.42
Individuals infected with mpox can also shed virus in their respiratory tracts, even in the absence of lesions.43,44,45,46,47,48 A majority of patients (60 percent) were positive for mpox virus on oropharyngeal swabs.49 One study noted that most positive oropharyngeal swabs did not come from patients with visible lesions in the throat at the time of testing.50
Environmental contamination of surfaces unlikely to have been touched by patients was documented in a hospital.51 Samples that were positive for mpox virus included the air vent above the door between the bedroom and the bathroom, “suggesting non-contact contamination possibly via respiratory droplets or re-aerosolization from activities such as changing bed linen.”
This means that individuals infected with mpox can release viral particles when breathing, speaking, coughing, singing, or laughing. Respiratory symptoms, including cough and nasal congestion, can occur with a mpox infection.52 A primer on aerosol transmission of respiratory viruses published in the journal Science states:53
- Respiratory droplets and aerosols can be generated by various expiratory activities. Advances in aerosol measurement techniques, such as aerodynamic and scanning mobility particle sizing, have shown that the majority of exhaled aerosols are smaller than 5 μm, and a large fraction are <1 μm for most respiratory activities, including those produced during breathing, talking, and coughing. Exhaled aerosols occur in multiple size modes that are associated with different generation sites and production mechanisms in the respiratory tract.
- … Aerosols produced by an infected individual may contain infectious viruses, and studies have shown that viruses are enriched in small aerosols (<5 μm). The transport of virus-laden aerosols is affected by the physicochemical properties of aerosols themselves and environmental factors, including temperature, relative humidity, ultraviolet radiation, airflow, and ventilation. Once inhaled, virus-laden aerosols can deposit in different parts of the respiratory tract. Larger aerosols tend to be deposited in the upper airway; however, smaller aerosols, although they can also be deposited there, can penetrate deep into the alveolar region of the lungs.
- ... Although both aerosols and droplets can be produced by infected individuals during expiratory activities, droplets fall quickly to the ground or surfaces within seconds, leaving an enrichment of aerosols over droplets. The airborne pathway likely contributes to the spread of other respiratory viruses whose transmission was previously characterized as droplet driven.
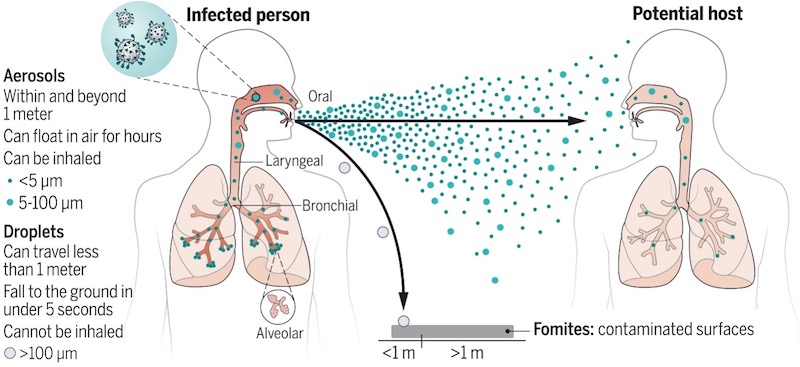
Image source: Wang, C.C., K.A. Prather, et al., “Airborne transmission of respiratory viruses,” Science, Aug 27, 2021.
Evidence from animal studies further elucidates airborne/aerosol transmission of the mpox virus. For example, studies conducted by U.S. Centers for Disease Control and Prevention (CDC) scientists found that caged prairie dogs infected with mpox infected others in separate nearby cages, and authors concluded that respiratory transmission is possible for mpox, though it may not occur at high rates.54,55
Studies have found that non-human primates can be systemically infected with the mpox virus when exposed via the respiratory tract to aerosols containing infectious virus and that there is no difference in systemic illness based on inoculation route.56,57,58,59 Another study cultured infectious virus from nasal discharge and oropharynx samples in prairie dogs up to 22 days after infection.60
In a 2003 outbreak related to infected prairie dogs in the United States, seven people were infected occupationally and had NOT handled a prairie dog, indicating airborne/aerosol transmission occurred.61 Five people reported having been within three feet of a prairie dog, one in the same room but not within three feet, and one person was in the same facility only within 48 hours of the death of an infected prairie dog.62
An outbreak at the Rotterdam Zoo indicates that aerosol transmission was likely at play.63 Giant anteaters became ill twelve days after arriving at the zoo. Subsequently, animals housed nearby but in separate cages became infected, including orangutans, African gorillas, chimpanzees, Asian gibbons, and others.
It is worth noting that, when airborne/aerosol transmission is possible, ruling out the role of airborne/aerosol transmission requires extensive contact tracing and data collection. For example, a recently published case report of a 20-year-old male demonstrated mpox infection without sexual exposure and with both possible contact and airborne exposures. The patient developed symptoms and tested positive for mpox about 14 days after attending a large, outdoor crowded event in the U.K. The patient did not wear a mask or a respirator during the event. No sexual contact was reported during his travel or in the preceding three months. The crowded event was the largest exposure risk for the individual, where transmission could have occurred via close contact or airborne/aerosol transmission. The report also notes that transmission could have occurred via fomites in a hotel or through any route during travel.64
Unanswered questions:
- How often does the mpox virus transmit via airborne/aerosol transmission?
- How much virus do people with mpox emit via respiratory events such as breathing, speaking, and coughing?
- Can the mpox virus be transmitted by people who are infected but who have not yet developed or who do not experience symptoms?
Transmission in the Absence of Symptoms
Main points:
- Asymptomatic mpox infections have been documented, but it is not clear how often they occur or whether or how often transmission can result.
- Some individuals with mpox may shed virus before or after lesions and other symptoms occur, but it is unclear whether or how often transmission can result.
Asymptomatic mpox infections have been documented, however, it is unclear how common asymptomatic mpox infections are. Three asymptomatic cases were identified in previously smallpox-vaccinated individuals after exposure to mpox-infected prairie dogs.65
Asymptomatic cases have also been identified during the ongoing 2022 mpox outbreak. One study in Belgium found evidence of asymptomatic infections in three individuals that had positive anorectal mpox PCR results after retrospective sexually transmitted infection (STI) screening.66
Another study also found mpox virus in anorectal swabs in asymptomatic individuals collected as part of a routine STI screening in France. Of the 200 asymptomatic individuals who were screened and were negative for N. gonorrhoeae and C. trachomatis, 6.5 percent were PCR positive for mpox, two of whom later developed symptoms.67
Transmission from asymptomatic mpox cases has not yet been documented. Contact tracing has been limited during the 2022 global outbreak, which means that data required to study asymptomatic transmission is not being effectively gathered. Some scientists hypothesize that asymptomatic transmission could be an explanation for why the virus has begun to spread so much more rapidly between humans compared to prior outbreaks.68
The CDC currently states that the infectious period begins with the onset of rash and ends when all scabs have fallen off and a fresh layer of intact skin as formed.69 Data on this topic is extremely limited. Epidemiologic data indicates that only a proportion of cases in the current outbreak are experiencing a prodrome prior to rash.70 Some data indicates that viral shedding may begin prior to symptom onset and/or continue after lesions have healed.71 Researchers found that Cynomolgus Macaques shed mpox virus in nasal and oral swabs concomitantly even prior to the presence of lesions – which suggests that humans infected with mpox could also shed or transmit the virus prior to showing clinical signs.72
Other studies have detected virus in multiple body fluids, such as saliva, blood, and semen, and lesions for four to 16 days after symptom onset.73 One study reported that a patient was negative on lesion swabs but positive on oropharyngeal, anal, and plasma samples on day five after symptom onset.74
Unanswered questions:
- How frequently do asymptomatic infections occur?
- Can transmission happen from asymptomatic infections? How often? Under what circumstances?
- Can transmission occur before onset of symptoms? How often and through what routes/body fluids?
- Can transmission occur after lesions have healed? How often and through what routes/body fluids?
Other Transmission Modes
Main points:
- Sexual transmission may be occurring with mpox, though it is unclear whether or how often at this point.
- Mpox virus has been detected in multiple body fluids (blood, saliva, semen, and vaginal fluid), but it is unclear whether or how often transmission can occur via these routes.
- The presence of genital lesions does not necessarily indicate site of inoculation.
- Maternal-to-fetal transmission and negative outcomes have been documented, though not much is known about mpox virus and pregnancy.
- Ocular transmission may be possible.
Sexual Transmission
The ongoing 2022 mpox outbreak in the United States has disproportionately affected gay, bisexual, and other men who have sex with men. Chains of transmission have been identified largely through sexual contact among men who have sex with men.75 Mpox virus particles have been detected in bodily fluids, such as blood, saliva, semen, and vaginal fluid.76 A study from Spain found high viral loads in most skin pustules, saliva, rectal swabs, semen, urine, and fecal samples from mpox cases.77 Another study isolated infectious mpox virus from a semen sample of an infected patient living with HIV, and the authors concluded, “semen collected in the acute phase of infection (day 6 after symptom onset) might contain a replication-competent virus and represent a potential source of infection.”78 While sexual transmission is a common or even predominant mode of transmission for the mpox virus, it is hard to rule out contact and airborne transmission during sexual interactions and thus these transmission modes must not be ignored as the clinical presentation of the virus can manifest in various ways.
Maternal-to-Fetal Transmission
Data on maternal mpox virus infection are limited, including susceptibility to or severity of disease. However, adverse pregnancy outcomes have been reported, including congenital mpox virus infection, spontaneous miscarriage, and fetal death.79,80 A 2017 study demonstrated generalized lesions on a stillborn fetus and high viral loads detected in several fetal tissues (umbilical cord and placenta),81 confirming vertical transmission of mpox virus during pregnancy or to the newborn by close contact during and after birth.82
Ocular Transmission
Ocular exposure to mpox virus may also be a potential route of transmission. Mpox lesions on eyelids and conjunctiva have been documented both prior to and during the 2022 outbreak.83,84,85 One study found similar viral loads on conjunctival and eye secretions compared with cutaneous lesions from a mpox-infected individual,86 raising the possibility of transmission through ocular secretions.
Unanswered questions:
- What body fluids can transmit the mpox virus? Under what circumstances and how often?
- What are the risk factors for and impacts of the mpox virus on pregnancy?
- Can inoculation occur through the eye?
Additional Considerations for Transmission
Main points:
- Certain conditions can increase the risk of infection and/or severe disease with mpox.
- The route of inoculation may influence severity of illness, though there is limited data on this topic.
- Co-infection with other pathogens can increase the risk of infection and/or severe disease with mpox.
- Vaccination may decrease the risk of infection.
Conditions that Can Increase Risk of Infection and/or Severe Disease with Mpox
Mpox virus can enter the body through broken skin (bodily fluids), mucous membranes (eyes, nose, or mouth), or the respiratory tract. Because of this, individuals with a history of atopic dermatitis (or eczema) and other skin conditions may be at increased risk of severe mpox disease.87
Route of Inoculation May Influence Severity of Illness
Route of orthopoxvirus infection, such as smallpox and mpox, may influence the clinical manifestations and severity of disease. For example, a 2012 review of smallpox transmission found that dermal and nasal exposures tended to produce less extensive spread of smallpox around the body compared with infection via lower respiratory tract deposition.88 Similarly, severe inflammation of the lung was observed in a 2011 study of Cynomolgus Macaques infected with mpox virus, suggesting that the lung is a major target organ of the virus.89 researchers also found that Cynomolgus Macaques shed mpox virus in nasal and oral swabs concomitantly even prior to the presence of lesions – which suggests that humans infected with mpox could also shed or transmit the virus prior to showing clinical signs.1
A 2006 study of human mpox cases associated with mpox-infected prairie dogs found that individuals who had been bitten or scratched by the animals experienced more pronounced systemic symptoms and were significantly more likely to have been hospitalized compared with those who had noninvasive exposures (e.g., touched an infected animal, cleaned an infected animal’s cage, and/or stood within 6 feet of an infected animal).90
Co-Infections with Other Pathogens
Evidence of co-infections with other pathogens have been documented and can also impact clinical severity. A case report in Germany documented a severe mpox virus infection of a 40-year-old patient who was concomitantly infected with syphilis and advanced HIV infection, with mpox lesions on the nasal area that progressed to necrosis.91 Given the ongoing, unabated Covid-19 pandemic around the world, individuals infected with mpox could also be co-infected with SARS-CoV-2. Researchers recently reported on a Covid-vaccinated patient who tested positive for mpox virus, SARS-CoV-2, and HIV infection. Notably, despite resolution of symptoms, the patient’s mpox oropharyngeal swab still tested positive after 20 days, suggesting that mpox-infected individuals may still be contagious for several days even after remission of symptoms.92 Additionally, the impacts of long Covid or post-acute Covid-19 syndrome (PASC) dysregulating the immune system could place some individuals at higher risk of mpox infection with an exposure and/or more severe disease.93
Mpox Vaccination
The JYNNEOS vaccine has been approved for the prevention of mpox and smallpox. The vaccine is administered in two doses 28 days apart.94 In the United States, t is recommended for people with sexual risk factors for mpox who have not been diagnosed with mpox (see risk factors here). The vaccine can also be administered in the two weeks following an identified exposure to mpox.
ACAM2000 vaccine is administered as a single dose by the percutaneous route using the multiple puncture technique. ACAM2000 vaccine is contraindicated for persons with atopic dermatitis or eczema, an immunocompromising condition (e.g., HIV), pregnancy, breastfeeding, and known underlying heart disease because of the risk for severe adverse effects resulting from the spread of vaccinia virus. 95
Vaccination can lower the risk of getting infected with mpox when exposed to the virus. Studies estimate the effectiveness of JYNNEOS at 66 to 89 percent with two doses and 36 to 75 percent with one dose. Meaning that, for example, with two doses, the chance of getting infected after exposure is 66 to 89 percent lower than people who are unvaccinated.96 The efficacy of the ACAM2000 vaccine against mpox infection is currently unknown as it has not been used in the ongoing 2022 mpox outbreak.97
1. Ježek et al., “Human Monkeypox: Clinical Features of 282 Patients,” The Journal of Infectious Diseases, August 1987.
2. Patrono, L.V., Pléh, K., Samuni, L. et al. Monkeypox virus emergence in wild chimpanzees reveals distinct clinical outcomes and viral diversity. Nat Microbiol 5, 955–965 (2020).
3. Khodakevich, L., Jezek, Z. & Kinzanzka, K. Isolation of monkeypox virus from wild squirrel infected in nature. Lancet 327, 98–99 (1986).
4. Radonić, A., S. Metzger, et al., “Fatal monkeypox in wild-living sooty mangabey, Cote d’Ivoire, 2012,” Emerging Infectious Diseases, June 2014.
5. Guarner, J., B.J. Johnson, et al., “Monkeypox transmission and pathogenesis in prairie dogs.” Emerging Infectious Diseases, March 2004.
6. U.K. Health Security Agency, "Qualitative assessment of the risk to the UK human population of monkeypox infection in a canine, feline, mustelid, lagomorph or rodent UK pet," Updated May 27, 2022.
7. Spickler, Anna Rovid, “Monkeypox Technical Factsheet,” The Center for Food Security & Public Health, August 2022.
8. Patrono, L.V., K. Pléh, et al. Monkeypox virus emergence in wild chimpanzees reveals distinct clinical outcomes and viral diversity. Nat Microbiol 5, 955–965 (2020).
9. Nigeria Centre for Disease Control, “National Monkeypox Public Health Response Guidelines,” 2019 (Accessed August 19, 2022).
10. Croft, D.R., M.J. Sotir, et al., “Occupational Risks during a Monkeypox Outbreak, Wisconsin, 2003,” Emerging Infectious Diseases, August 2007.
11. Learned, L.A., M.G. Reynolds, et al., “Extended Interhuman Transmission of Monkeypox in a Hospital Community in the Republic of the Congo, 2003,” The American Journal of Tropical Medicine and Hygiene Am J Trop Med Hyg 73.2 (2005): 428-434.
12. Vaughan, A., E. Aarons, et al., “Two cases of monkeypox imported to the United Kingdom, September 2018,” Eurosurveillance, September 20, 2018.
13. Jezek, Z., I. Arita, et al. “Four generations of probable person-to-person transmission of human monkeypox.” American Journal of Epidemiology vol. 123,6 (1986): 1004-12.
14. Yinka-Ogunleye, A., O. Aruna, et al., “Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report,” The Lancet Infectious Diseases, July 5, 2019.
15. Adler, H., S. Gould, et al., “Clinical features and management of human monkeypox: a retrospective observational study in the UK,” Lancet Infectious Diseases, Aug 1, 2022.
16. Seang, S., S. Burrel, et al., “Evidence of human-to-dog transmission of monkeypox virus,” The Lancet, August 10, 2022.
17. Thornhill, J.P., S. Barkati, et al., “Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022,” NEJM, July 21, 2022, DOI: 10.1056/NEJMoa2207323.
18. Tarín-Vicente, E.J., A. Alemany, et al., “Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study,” The Lancet, Aug 8, 2022.
19. Veintimilla, C., P. Catalán, et al., “The relevance of multiple clinical specimens in the diagnosis of monkeypox virus, Spain, June 2022,” Eurosurveillance, August 2022.
20. Pittman, P.R., J.W. Martin, et al., “Clinical characterization of human monkeypox infections in the Democratic Republic of the Congo,” medRxiv, May 2022.
21. Essbauer, S., H. Meyer, et al., “Long-lasting stability of vaccinia virus (orthopoxvirus) in food and environmental samples,” Zoonoses Public Health, 2007, doi: 10.1111/j.1863-2378.2007.01035.x.
22. Morgan, C.N., F. Whitehill, et al., “Environmental Persistence of Monkeypox Virus on Surfaces in Household of Person with Travel-Associated Infection,” Dallas, Texas, USA, 2021, Emerging Infectious Diseases, August 2022.
23. Atkinson, B., C. Burton, et al., “Infection-competent monkeypox virus contamination identified in domestic settings following an imported case of monkeypox into the UK,” Environmental Microbiology, July 2022.
24. Pfeiffer, J.A., A. Collingwood, et al., “High-Contact Object and Surface Contamination in a Household of Persons with Monkeypox Virus Infection — Utah, June 2022,” MMWR Early Release, August 2022.
25. Gould, S., B. Atkinson, et al., “Air and surface sampling for monkeypox virus in UK hospitals,” medRxiv, July 2022.
26. Nörz, D., S. Pfefferle, et al., “Evidence of surface contamination in hospital rooms occupied by patients infected with monkeypox, Germany, June 2022,” Eurosurveillance, 27(36), June 2022.
27. Reynolds, M.G., W.B. Davidson, et al., “Spectrum of Infection and Risk Factors for Human Monkeypox, United States, 2003,” Emerging Infectious Diseases, September 2007.
28. Verreault, D., S.Z. Killeen, et al., “Susceptibility of monkeypox virus aerosol suspensions in a rotating chamber,” Journal of Virological Methods,” February 2013.
29. Gould, S., B. Atkinson, et al., “Air and surface sampling for monkeypox virus in UK hospitals,” medRxiv, July 2022.
30. Vaughan, A., E. Aarons, et al., “Human-to-Human Transmission of Monkeypox Virus, United Kingdom, October 2018,” Emerging Infectious Diseases, February 2020.
31. Bunge, E.M., B. Hoet, et al., “The changing epidemiology of human monkeypox—A potential threat? A systematic review,” PLoS Neglected Tropical Diseases, February 2022https://doi.org/10.1371/journal.pntd.0010141.
32. Therkorn, J., D. Drewery, et al., “Development and Comparison of Complementary Methods to Study Potential Skin and Inhalational Exposure to Pathogens During Personal Protective Equipment Doffing,” Clinical Infectious Diseases, 2019.
33. Milton, D.K. “What was the primary mode of smallpox transmission? Implications for biodefense,” Frontiers in Cellular and Infection Microbiology vol. 2 150. 29 Nov. 2012.
34. Airborne transmission of smallpox. (1970). British medical journal, 4(5728), 127.
35. Behbehani A. M. (1983). The smallpox story: life and death of an old disease. Microbiological reviews, 47(4), 455–509.
36. Ontario Agency for Health Protection and Promotion (Public Health Ontario). Infection prevention and control (IPAC) recommendations for monkeypox in health care settings. Toronto, ON: Queen’s Printer for Ontario; 2022.
37.U.S. Centers for Disease Control and Prevention, “Clinical Recognition,” last updated August 5, 2022.
38.Thornhill, J.P., S. Barkati, et al., “Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022,” New England Journal of Medicine, July 2022, DOI: 10.1056/NEJMoa2207323.
39.Tarín-Vicente, E.J., A. Alemany, et al., “Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study,” The Lancet, August 2022.
40. Erez, N., H. Achdout, et al., “Diagnosis of Imported Monkeypox, Israel, 2018,” Emerging Infectious Diseases, March 2019.
41.Pittman, P.R., J.W. Martin, et al., “Clinical characterization of human monkeypox infections in the Democratic Republic of the Congo,” medRxiv, May 2022
42.Thornhill, J.P., S. Barkati, et al., “Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022,” New England Journal of Medicine, July 2022, DOI: 10.1056/NEJMoa2207323.
43. Adler, H., S. Gould, et al., “Clinical features and management of human monkeypox: a retrospective observational study in the UK,” The Lancet Infectious Diseases, August 2022.
44. Karan, A., A.R., Styczynski, et al., “Human Monkeypox without Viral Prodrome or Sexual Exposure, California, USA, 2022,” Emerging Infectious Diseases, August 15, 2022.
45. Allan-Blitz, L.T., K. Carragher, et al., “Laboratory Validation and Clinical Implementation of Human Monkeypox Saliva-Based Tests,” medRxiv, August 2022.
46. Thornhill, J.P., S. Barkati, et al., “Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022,” New England Journal of Medicine, July 2022, DOI: 10.1056/NEJMoa2207323.
47. Tan, D.H.S., S. Jaeranny, et al., “Atypical clinical presentation of monkeypox complicated by myopericarditis,” Open Forum Infectious Diseases, August 2022.
48. Guarner, J., B.J. Johnson, et al., “Monkeypox Transmission and Pathogenesis in Prairie Dogs,” Emerging Infectious Diseases, March 2004.
49. Tarín-Vicente, E.J., A. Alemany, et al., “Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study,” The Lancet, August 2022.
50.Veintimilla, C., P. Catalán, et al., “The relevance of multiple clinical specimens in the diagnosis of monkeypox virus, Spain, June 2022,” Eurosurveillance, August 2022.
51. Gould, S., B. Atkinson, et al., “Air and surface sampling for monkeypox virus in UK hospitals,” medRxiv, July 21, 2022.
52. U.S. Centers for Disease Control and Prevention, “Monkeypox: Signs and Symptoms,” Updated Aug 5, 2022, Available at (Accessed Aug 19, 2022).
53. Wang, C.C., K.A. Prather, et al., “Airborne transmission of respiratory viruses,” Science, Aug 27, 2021.
54. Hutson, C.L., N. Gallardo-Romero, et al., “Transmissibility of the Monkeypox Virus Clades via Respiratory Transmission: Investigation Using the Prairie Dog-Monkeypox Virus Challenge System,” PLOS ONE, Feb 7, 2013.
55. Hutson, C.L., D.S. Carroll, et al., “Monkeypox disease transmission in an experimental setting: prairie dog animal model,” PLoS One, 2011, 6(12): e28295, https://doi.org/10.1371/journal.pone.0028295.
56. Goff, A.J., J. Chapman, et al., “A Novel Respiratory Model of Infection with Monkeypox Virus in Cynomolgus Macaques,” Journal of Virology, April 2011.
57. Barnewall, R.E., D.A. Fisher, et al., “Inhalational monkeypox virus infection in cynomolgus macaques,” Frontiers in Cellular and Infection Microbiology, September 2012.
58. Johnson, R.F., J. Dyall, et al., “Comparative Analysis of Monkeypox Virus Infection of Cynomolgus Macaques by the Intravenous or Intrabronchial Inoculation Route,” J Virology, 2011, 85(5).
59. Barnewall, R.E., D.A. Fisher, et al., “Inhalational monkeypox virus infection in cynomolgus macaques,” Front Cell Infect Microbiol, 2012.
60. Xiao, S.Y., E. Sbrana, et al., “Experimental Infection of Prairie Dogs with Monkeypox Virus,” Emerging Infectious Diseases, April 2005.
61. Croft, D. R., Sotir, et al. (2007). Occupational risks during a monkeypox outbreak, Wisconsin, 2003. Emerging infectious diseases, 13(8), 1150–1157.
62. Ibid.
63. Parker, S. and R.M. Buller, “A review of experimental and natural infections of animals with monkeypox virus between 1958 and 2012,” Future Virol, 2013, 8(2): 129-157.
64. Karan, A., A.R. Styczynski, et al., “Human Monkeypox without Viral Prodrome or Sexual Exposure, California, USA, 2022,” Emerging Infectious Diseases, August 15, 2022.
65. Hammarlund, E., M.W. Lewis, et al., “Multiple diagnostic techniques identify previously vaccinated individuals with protective immunity against monkeypox,” Nature Medicine, August 2005.
66. De Baetselier, I., C. Van Dijck, et al., “Asymptomatic monkeypox virus infections among male sexual health clinic attendees in Belgium,” medRxiv, July 2022.
67. Ferré, V.M., A. Bachelard, et al., “Detection of Monkeypox Virus in Anorectal Swabs From Asymptomatic Men Who Have Sex With Men in a Sexually Transmitted Infection Screening Program in Paris, France,” Annals of Internal Medicine, August 2022.
68. De Baetselier, I., C. Van Dijck, et al., “Asymptomatic Monkeypox Virus Infections Among Male Sexual Health Clinic Attendees in Belgium,” Preprints with the Lancet, June 21, 2022.
69. U.S. CDC, “Clinician FAQs: Monkeypox Transmission, Risk, and Strains, When is someone with monkeypox contagious?” Updated Aug 11, 2022, Available at (Accessed Aug 22, 2022).
70. Thornhill, J.P., S. Barkati, et al., “Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022,” NEJM, July 21, 2022.
71. Adler, H., S. Gould, et al., “Clinical features and management of human monkeypox: a retrospective observational study in the UK,” The Lancet Infectious Diseases, Aug 1, 2022.
72. Johnson, R.F., J. Dyall, et al., “Comparative Analysis of Monkeypox Virus Infection of Cynomolgus Macaques by the Intravenous or Intrabronchial Inoculation Route,” Journal of Virology, February 2011.
73. Peiro-Mestres, A., I. Fuertes, et al., “Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022,” Eurosurveillance, July 2022, link.
74. Veintimilla, C., P. Catalán et al., “The relevance of multiple clinical specimens in the diagnosis of monkeypox virus, Spain, June 2022,” Eurosurveillance, August 2022.
75. Leonard, C.M., K. Poortinga, et al., “Mpox Outbreak — Los Angeles County, California, May 4–August 17, 2023,” MMWR, January 18, 2024.
76. Tan, D.H.S., S. Jaeranny, et al., “Atypical clinical presentation of monkeypox complicated by myopericarditis,” Open Forum Infectious Diseases, August 2022.
77. Peiró-Mestres, A., I. Fuertes, et al., “Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022,” Eurosurveillance, July 2022.
78. Lapa, D., F. Carletti, et al., “Monkeypox virus isolation from a semen sample collected in the early phase of infection in a patient with prolonged seminal viral shedding,” The Lancet Infectious Diseases, August 2022.
79. Mbala, P.K., J.W. Huggins, et al., “Maternal and Fetal Outcomes Among Pregnant Women With Human Monkeypox Infection in the Democratic Republic of Congo,” The Journal of Infectious Diseases, October 2017.
80. Meaney-Delman, D.M., R. Galang, “A Primer on Monkeypox Virus for Obstetrician–Gynecologists: Diagnosis, Prevention, and Treatment,” Obstetrics & Gynecology,2022, 140(3):391-397 doi: 10.1097/AOG.0000000000004909.
81. Mbala, P.K., J.W. Huggins, et al., “Maternal and Fetal Outcomes Among Pregnant Women With Human Monkeypox Infection in the Democratic Republic of Congo,” The Journal of Infectious Diseases, October 2017.
82. U.S. Centers for Disease Control and Prevention, “Clinical Considerations for Monkeypox in People Who are Pregnant or Breastfeeding,” last updated July 18, 2022.
83. Benatti, S.V., S. Venturelli, et al., “Ophthalmic manifestation of monkeypox infection,” July 2022, The Lancet Infectious Diseases.
84. Hughes, C., A. McCollum, et al., “Ocular complications associated with acute monkeypox virus infection, DRC,” International Journal of Infectious Diseases, April 2014.
85. Ježek, Z., M. Szczeniowski, et al., “Human Monkeypox: Clinical Features of 282 Patients,” The Journal of Infectious Diseases, August 1987.
86. Meduri, E., A. Macles, et al., “Conjunctivitis with Monkeypox Virus Positive Conjunctival Swabs,” Ophthalmology, August 2022.
87. U.S. Centers for Disease Control and Prevention, “Clinical Considerations for Monkeypox in Children and Adolescents,” last updated August 22, 2022.
88. Milton, D., “What was the primary mode of smallpox transmission? Implications for biodefense,” Frontiers in Cellular and Infection Microbiology, November 2012.
89. Johnson, R.F., J. Dyall, et al., “Comparative Analysis of Monkeypox Virus Infection of Cynomolgus Macaques by the Intravenous or Intrabronchial Inoculation Route,” Journal of Virology, February 2011.
90. Reynolds, M.G., K.L. Yorita, et al., “Clinical Manifestations of Human Monkeypox Influenced by Route of Infection,” The Journal of Infectious Diseases, September 2006.
91. Boesecke, C., M.B. Monin, et al., “Severe monkeypox-virus infection in undiagnosed advanced HIV infection,” Infection, August 2022.
92. Nolasco, S., F. Vitale, et al., “First case of monkeypox virus, SARS-CoV-2 and HIV co-infection,” Journal of Infection, August 2022.
93. Proal AD and VanElzakker MB (2021) Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms. Front. Microbiol. 12:698169. doi: 10.3389/fmicb.2021.69816994. U.S. Centers for Disease Control and Prevention, “Mpox Vaccine Recommendations,” Last updated April 22, 2024.
94. U.S. Centers for Disease Control and Prevention, “Mpox Vaccine Recommendations,” Last updated April 22, 2024.
95. Rao et al., “Use of JYNNEOS (Smallpox and Monkeypox Vaccine, Live, Nonreplicating) for Preexposure Vaccination of Persons at Risk for Occupational Exposure to Orthopoxviruses: Recommendations of the Advisory Committee on Immunization Practices — United States, 2022,” MMWR Early Release, June 2022
96. U.S. Centers for Disease Control and Prevention, “Jynneos Vaccine Effectiveness,” Last updated May 18, 2023.
97. U.S. Centers for Disease Control and Prevention, “Mpox: Vaccination,” last updated August 2024.