NNU Infectious Diseases Survey: November 2024 Preliminary Results
Health care facility infectious disease protections are inadequate, jeopardize health care worker and patient health and safety.
National Nurses United (NNU), the largest and fastest growing labor union and professional association for registered nurses (RNs) in the United States, is conducting a survey of RNs regarding infection prevention practices related to a range of infectious diseases at health casre facilities across the nation. Preliminary results include responses from 496 RNs who work in 41 states and DC, including both NNU members and non-union RNs. Preliminary results were collected between October 11 and 30, 2024; the survey remains open and final results are pending.
Screening and Isolation of Infectious/Potentially Infectious Patients
It is essential for health care facilities to have protocols in place to screen patients and visitors to effectively identify individuals who are or may be infectious. Accurate and timely identification of infectious/potentially infectious patients is essential to ensure isolation, which is a key part of preventing exposure and transmission.
NNU's preliminary survey results indicate that many health care employers are failing to consistently screen and isolate patients who are or may be infectious:
- More than half of RNs (55.4 percent) report that patients are inconsistently or never screened for respiratory infectious diseases at the point of entry to their health care facility, including TB, influenza, Covid-19, and RSV. Only 37.1 percent of RNs report that patients are always or often screened.
- Only about half of RNs (49.2 percent) report that their facility always isolates patients who have or might have a respiratory infectious disease.
- When it comes to novel pathogens, education and proactive screening are essential to combat outbreaks and protect health care workers and patients. Yet, only 20.4 percent of RNs report that their employer has provided information about the novel avian influenza virus and how to recognize, screen, and respond to possible cases.
Ventilation is an important part of effectively preventing transmission of infectious particles through the air, including both use of airborne infection isolation rooms (AIIRs) and providing ventilation and filtration in patient care and other areas of the facility.
NNU's preliminary survey results find a significant lack of attention to ventilation:
- Less than half of RNs (41.9 percent) report that AIIRs or negative pressure rooms are used to isolate infectious patients at their facility.
- Nearly a third of RNs (31.7 percent) were not sure about the types of ventilation and air cleaning measures their employers had implemented, which underlines the lack of planning and communication from employers about these important issues.
- Only a small proportion of RNs report that their employers had implemented other, proven measures to improve air hygiene: higher ventilation rates than minimally required (4.8 percent); higher filtration level for recirculated air than minimally required (5.6 percent); additional rooms and/or entire units have been converted to negative pressure isolation (8.9 percent); portable HEPA filters are utilized (16.7 percent).
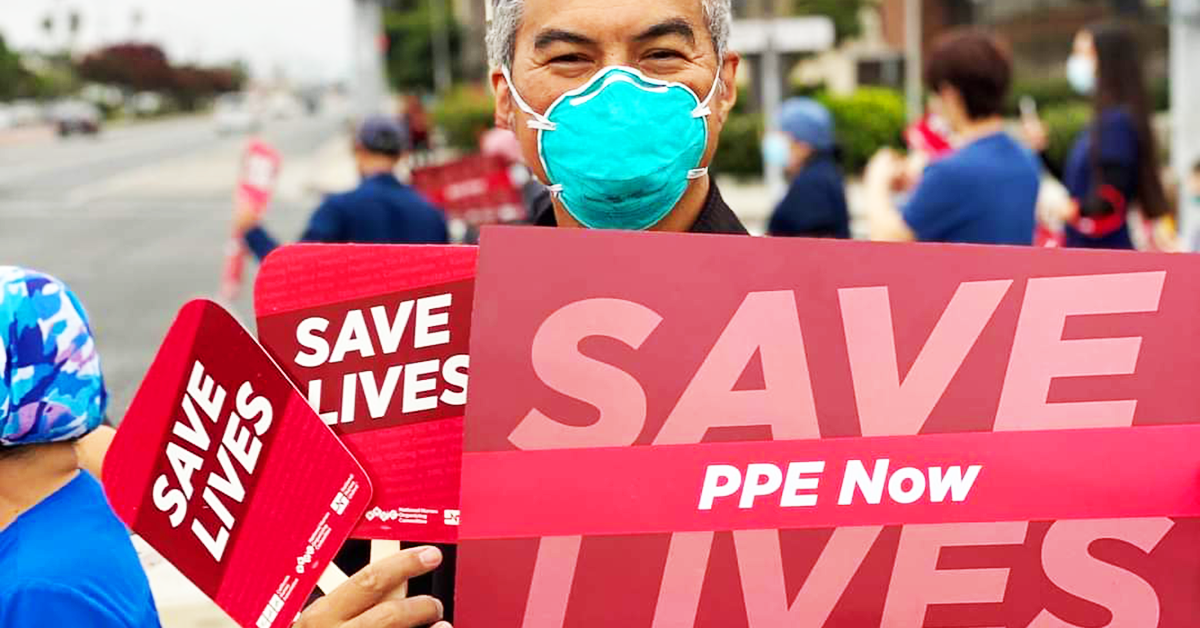
Personal Protective Equipment (PPE)
PPE, which should be used in the context of the hierarchy of controls, is an essential element of protection for health care workers. Nurses and other health care workers frequently provide hands on care to infectious/potentially infectious patients, which necessitates being near an infectious source for long periods of time. PPE can reduce these risks of transmission to health care workers. Different types of PPE, such as respirators approved by the National Institute for Occupational Safety and Health (NIOSH), eye protection, isolation gowns, coveralls, and gloves, are used and must be selected based upon a pathogen's transmission route(s) and an exposure assessment.
NNU's preliminary survey reveals significant issues in health care facilities' current PPE practices:
- For three major aerosol-transmissible diseases — TB, measles, and Covid — RNs report inadequate PPE use. Respirators should be used for each of these pathogens, but only 65.3 percent of RNs report that their health care facility uses a respirator for TB, only 36.1 percent for measles, and only 63.5 percent for Covid-19.
- For Covid-19, nearly half of RNs (49.8 percent) report that their facility uses a surgical mask. This is extremely concerning because the evidence is clear that SARS-CoV-2/Covid-19 is aerosol-transmitted and a NIOSH-approved respirator is required to protect health care workers from exposure. A surgical mask does not provide respiratory protection.
- Nearly half of RNs (49.0 percent) are not sure what PPE their facility uses for avian (novel) influenza, which indicates a severe lack of preparedness by health care employers.
- Only 60.5 percent of RNs have access to sufficient supply of N95s or other kinds of respirators on their unit. Access is key to RNs and other health care workers being able to deploy PPE when it is necessary to protect their health and safety.
- More than one in six RNs (18.4 percent) have not been fit tested in the previous year.
- RNs are still being required to reuse PPE designed for single use, which is an unacceptable and dangerous practice. Only 68.8 percent of RNs report they do not reuse any single use PPE. Nearly one in five RNs (18.8 percent) report that they are still required to reuse single-use N95 respirators — a practice that has been shown to leave health care workers unprotected. Reuse of single-use PPE leaves health care workers unprotected.
Policies for Mask Use for Source Control
Source control — the idea of limiting infectious emissions at the source to prevent them from entering a share airspace in order to reduce the chance of onward transmission — is an important element in preventing infectious disease spread in health care settings. In addition to screening and prompt isolation of infectious/potentially infectious patients, masks can be used for source control. There is growing evidence regarding the effectiveness of masks for reducing infectious respiratory emissions from the wearer and limiting onward transmission, especially when universal masking is employed.
NNU's preliminary survey results show that mask use for source control is inconsistent across health care facilities:
- The most common mask policies reported by RNs are voluntary only (35.5 percent), followed by universal masking only during periods of high transmission (29.4 percent) and masking is only required in certain units (14.3 percent). Just 10.8 percent of RNs report that their facility uses universal masking at all times for source control.
Exposure Tracking & Notification
Notifying health care workers of workplace exposures to infectious diseases is important because it enables timely monitoring for infection, which can be key for preventing onward transmission to others. Tracking infectious disease exposures is an essential part of evaluating the effectiveness of an employer's infection prevention program. Exposure notification is also essential to enabling workers to connect infections to occupational exposures, which can enable access to workers compensation and other benefits and supports.
NNU's preliminary survey results indicate that health care employers are not effectively tracking and notifying health care workers of exposures to infectious diseases:
- More than half of RNs (64.5 percent) report inconsistent, infrequent, or non-existent notification from their employers regarding infectious disease exposures.
- Only 24.7 percent of RNs report that their employer always notifies them of exposures to infectious diseases in a timely fashion.
Work-Related Infections and Time Off Work to Recover
When health care employers fail to implement protective measures, such as patient screening and isolation, PPE, source control, and exposure notification, health care workers are placed at increased risk of exposure and infection to a variety of infectious agents.
More than half of RNs (57.5 percent) have sustained at least one infectious disease from work, including the common cold, influenza, Covid-19, and MRSA.
NNU's preliminary survey results illuminate the significant impacts of work-related infections:
- The vast majority of RNs report taking time off work to recover from an infection sustained at work. About half of RNs (52.3 percent) took up to one week off work to recover. A substantial proportion of RNs (41.9 percent) required more than one week off work to recover.
- For RNs who took time off work to recover from a work-related infection, only a small proportion (16.4 percent) were provided additional paid time or workers compensation while they recovered. Most RNs were expected to use their own sick time (34.2 percent), their paid time off (PTO) bank (29.7 percent), or their own vacation time (3.7 percent) while they recovered, even though the infection was sustained at work.
Long Covid
A significant proportion of RNs and other health care workers have been infected with Covid-19 because their employers provided inadequate protections. Data indicate that about one in six Covid-19 infections can result in ongoing, recurrent, or new symptoms known as long Covid. Long Covid can significantly impact an individual's ability to work and daily activities outside of work.
NNU's preliminary survey results indicate that RNs continue to experience significant impacts from long Covid:
- A majority of RNs report experiencing symptoms after recovery from Covid-19. Only 26.8 percent of RNs report no symptoms after recovery from initial infection.
- RNs report experiencing several symptoms of long Covid, including tiredness or fatigue (39.1 percent), memory or concentration difficulties (29.2 percent), joint or muscle pain (26.0 percent), headaches or migraines (19.4 percent), difficulty sleeping (17.5 percent), difficulty breathing or shortness of breath (13.1 percent), symptoms that get worse after physical or mental activities (11.7 percent), heart palpitations (9.7 percent), chest pain (4.8 percent)
- RN experiencing long Covid report long-lasting symptoms — 50 percent of RNs report long Covid symptoms lasting longer than six months.
- Most RNs required time off work due to long Covid symptoms — 25.2 percent of RNs were able to take the time off work they needed, 15.9 percent needed time off work but were unable to take all the time they needed, and 13.8 percent needed time off work but were unable to take any. A majority of RNs who took time off work due to long Covid took less than one month.
- A majority of RNs who experienced long Covid report their symptoms have affected their ability to work (73.5 percent) and their daily activities outside of work (86.9 percent).